Root canal treatment is a highly effective procedure designed to save a severely damaged or infected tooth. While the thought of undergoing a root canal may seem intimidating, knowing what to expect can ease any anxiety.
The treatment is often necessary when the pulp of a tooth becomes infected, usually due to decay, trauma, or a cracked tooth. The procedure involves cleaning out the infection and sealing the tooth to prevent further issues.
In this blog, we will walk through the five basic steps of a root canal, explain each phase in detail, and provide an understanding of what happens during this common dental procedure.
Root Canal: What Is It?
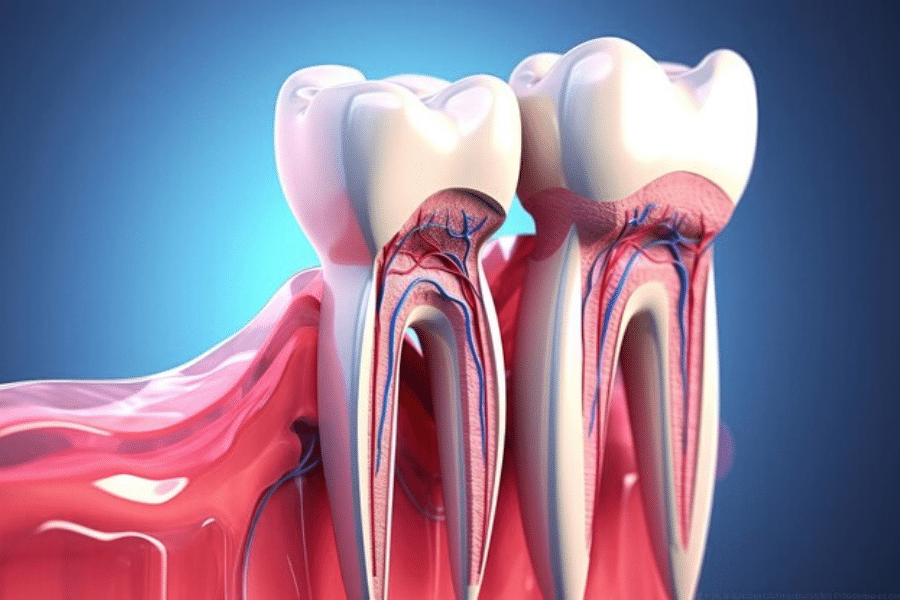
A root canal is a dental procedure that focuses on treating the inside of a tooth. Each tooth contains a soft tissue known as the pulp, which houses blood vessels, nerves, and connective tissues. If the pulp becomes infected or inflamed due to cavities, fractures, or trauma, it can cause pain and may eventually lead to tooth loss.
A root canal removes the damaged pulp and disinfects the tooth, preserving its structure and function. Now that we understand the basics, let’s break down the five steps involved in a root canal.
Step-by-Step Breakdown: 5 Basic Stages of a Root Canal
1. Diagnosis and Preparation
The first step in the root canal process is diagnosing the problem and preparing the patient for the procedure.
Key Steps in the Diagnosis Phase:
- Examination: The dentist examines the tooth in question and may perform diagnostic tests such as tapping the tooth or applying heat to determine sensitivity. An X-ray is usually taken to assess the extent of the infection or damage.
- Symptoms: Common symptoms that indicate the need for a root canal treatment include severe tooth pain, sensitivity to hot or cold, swelling, and tenderness in the gums.
- Numbing the Area: Once the dentist determines that a root canal is necessary, they will apply a local anesthetic to numb the affected tooth and surrounding tissues. This ensures the patient is comfortable throughout the procedure.
Once the patient is prepared and the tooth is numbed, the dentist begins the next step of the process.
2. Accessing The Pulp Chamber
The second step involves accessing the pulp chamber, the innermost part of the tooth where the infected or inflamed pulp resides.
Steps in Accessing the Tooth:
- Creating an Opening: The dentist uses a dental drill to create a small opening on the top (or back) of the tooth to access the pulp chamber.
- Isolation of the Tooth: To prevent saliva from contaminating the treatment area, the dentist places a rubber dam around the tooth. This keeps the tooth clean and dry during the procedure.
Opening the tooth gives the dentist direct access to the infected pulp, allowing them to move on to the next step, which is crucial to stopping the infection.
3. Removing The Infected Pulp
This is the most critical step of the root canal treatment, where the infected pulp tissue is completely removed from the tooth.
Steps in Cleaning the Tooth:
- Pulp Removal: Using specialized dental tools, the dentist carefully removes the damaged or infected pulp from the pulp chamber and root canals. This step eliminates the source of infection and pain.
- Shaping the Root Canals: Once the pulp is removed, the dentist uses small files to shape the root canals and ensure that all debris and infected tissue are cleared away. This preparation allows for proper filling in later stages.
Removing the infected pulp is essential to prevent the spread of infection and to preserve the natural tooth. After cleaning the canals, the dentist will disinfect the area to ensure that no harmful bacteria remain.
4. Cleaning and Disinfecting The Canals
After removing the infected pulp, the dentist thoroughly cleans and disinfects the tooth to eliminate any remaining bacteria.
Disinfection Process:
- Irrigation: The dentist flushes the root canals with an antiseptic solution to kill any remaining bacteria. This step is crucial to preventing reinfection.
- Drying the Canals: Once the dentist cleans and disinfects the canals, they carefully dry them to ensure no moisture remains inside the tooth. Moisture can contribute to further bacterial growth, so the canals need to be completely dry before sealing.
Thorough disinfection ensures the tooth is free of infection and ready for sealing. After this step, the dentist prepares the tooth for the final stages of the procedure.
5. Filling and Sealing The Tooth
The final step in the root canal process is to fill and seal the tooth to protect it from future infection and restore its function.
Sealing the Tooth:
- Filling the Canals: The dentist fills the cleaned root canals with a rubber-like material called gutta-percha. This material is biocompatible and seals the canals to prevent bacteria from re-entering the tooth.
- Temporary or Permanent Filling: Depending on the extent of the damage, the dentist may place a temporary filling over the tooth or, in some cases, a permanent filling. In most cases, the dentist uses a temporary filling and schedules a follow-up appointment for the final restoration.
- Placing a Crown: In many cases, the dentist recommends a dental crown to cover the tooth after a root canal. This provides additional protection and helps restore the tooth’s strength and function.
The dentist seals the tooth to fully protect it from future damage or infection. At this point, they complete the root canal, and the tooth is saved.
Tips for a Smooth Recovery After a Root Canal
Although a root canal is a relatively straightforward procedure, the recovery process is important for ensuring the success of the treatment. Here are a few tips to ensure a smooth recovery:
- Avoid hard or crunchy foods for a few days after the procedure.
- Take prescribed pain medications to manage any discomfort.
- To ensure proper dental health, practice consistent brushing and flossing.
- Attend follow-up appointments to monitor healing and receive the final restoration.
A root canal treatment may sound intimidating, but understanding the process can help ease any concerns. The dentist follows five basic steps—diagnosing and preparing, accessing the pulp chamber, removing the infected pulp, cleaning and disinfecting the canals, and sealing the tooth—to save your tooth and relieve pain caused by infection.
With modern dental technology and local anesthesia, the procedure is generally painless and highly effective. If you’re having symptoms such as severe tooth pain or sensitivity, it’s essential to consult your dentist to determine if a root canal is necessary.
By addressing the problem early, you can avoid more complex issues and preserve your natural teeth. Taking good care of your teeth after the procedure and following your dentist’s instructions will ensure a successful recovery and long-lasting results.





